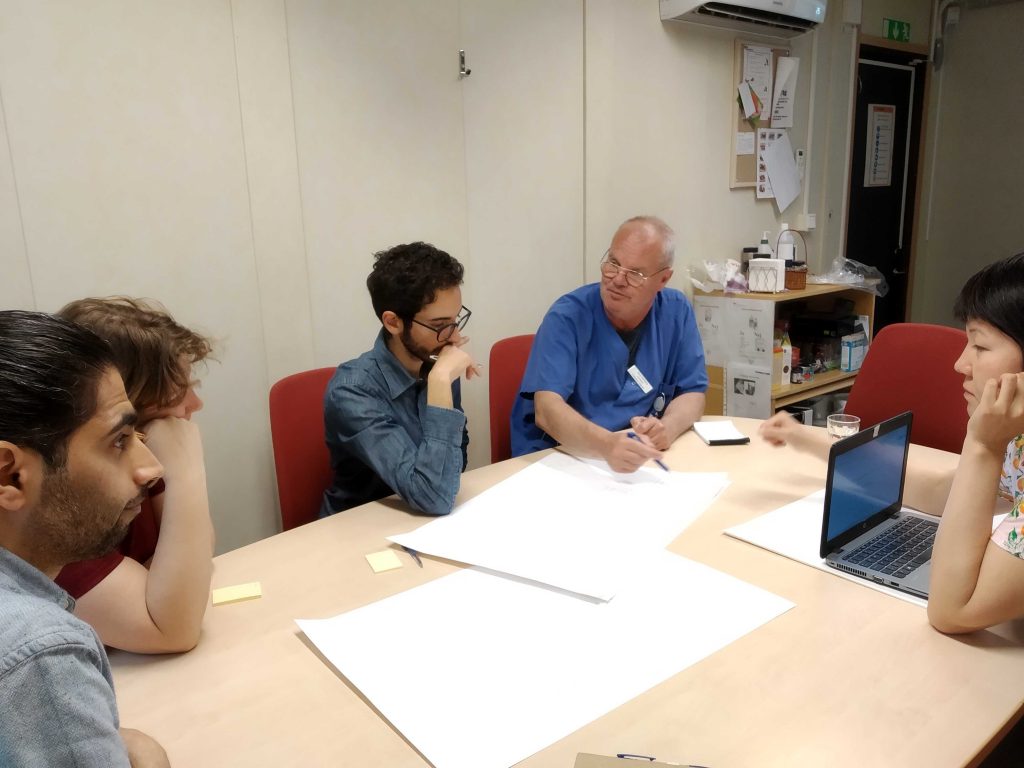
As part of RISE’s Clinical Innovation Fellowship, my team members and I were tasked to research the journey(s) of palliative patients and their caretakers in Lerum Kommun and Alingsås hospital. The purpose of the project was to understand the palliative patients’ experiences by including perspectives and needs of all stakeholders, while using Stanford’s BioDesign method. Looking into the lives of terminally ill people from human-centered perspective, while immersing into a clinical healthcare environment was an intimidating undertaking. My head was full of doubts and questions. Do I have enough courage to temper with the subject of death? How can I be both professional, strong and yet empathetic and respectful towards the life situation of palliative patients? What does need-driven innovation looks like in the field of palliative care?
I turned to what I know best, and that is ethnographic field research. It feels like solving a rewarding puzzle. While it takes a lot of time, identifying and categorizing piece by piece large amounts of research data from interviews, shadowing, meetings, and home visits, I am always curious and excited about meeting people. In our case, we were given unprecedented access to all the important stakeholders around palliative patients.
We met some incredible healthcare professionals who were open and engaged. Over the course of our immersion, we interviewed and observed the work of medical and non-medical personal at the Alingsås hospital and Lerum kommun (including dr., surgeon, assistant nurses, nurses, dietician, pharmacist, priest, and social workers). Most importantly, we talked to many patients themselves, whether at their own homes or elderly home facilities.
While one can never understand the existential loneliness and sorrow of a terminally ill person, we got pretty close to getting to know the primary stakeholders – spending days and nights at the hospital and elderly home, listening to their stories and seeing them at work. We saw small gestures of kindness – how nurses gently moved patients to avoid bed sores, held their hands to soothe anxiety or crushed pills to make them easier to swallow. The most memorable encounter was witnessing how an assistant nurse watched over the needs of a palliative patient during her last hours alive. She expressed nothing but love for the patient, taking every wrinkle, sigh and heavy, bubbly breath seriously until the very end. Extraordinary moment.
What I have learned from this immersion is that stakeholders around palliative patients are made of distinct professions attentending to the whole of a person. They might have complementary yet competing perspectives and priorities (i.e. medical vs. patient) which can be a challenge. Members from the same palliative team, for example, can have different understanding of and relationship to a patient, whether it is a dr. or a priest.
Team collaboration is a must in the palliative care, because the quality of collaboration directly affects patient care. Looking at all the stakeholders under the umbrella of the same project helps to identify gaps and barriers in the system (i.e. IT, law, priorities). The challenge is to identify needs and opportunities for improvement via perspectives of the palliative persons and their families though. Empathy becomes part of strategic criteria.
When meeting nurses and assistant nurses specifically, it was vital to be clear and transparent about the goals of our research project. We were there to listen and learn rather than inspect and criticize, I said many times to assistant nurse. It was equally important to show respect, remember people’s names and stay humble, which in return, helped to break the ice and get answers to crucial questions.
And I learned that the palliative care is about living rather than dying.
Amina Kadribasic
Team Gothenburg, CIF 2019










 The Golden Gate Bridge (Photo credits: Giampaolo)
The Golden Gate Bridge (Photo credits: Giampaolo) Frozen lake in Dalarna (Photo credits: Jenny)
Frozen lake in Dalarna (Photo credits: Jenny)



